Cell Surface and Functional Features of Cortical Bone Stem Cells
皮质骨干细胞的细胞表面和功能特征
The newly established mouse cortical-bone-derived stem cells (mCBSCs) are unique stem cells compared to mouse mesenchymal stem cells (mMSCs). The mCBSC-treated hearts after myocardial infarction have been reported to have greater improvement in myocardial structure and functions. In this study, we examined the stemness features, cell surface glycan profiles, and paracrine functions of mCBSCs compared with mMSCs. The stemness analysis revealed that the self-renewing capacity of mCBSCs was greater than mMSCs; however, the differentiation capacity of mCBSCs was limited to the chondrogenic lineage among three types of cells (adipocyte, osteoblast, chondrocyte). The cell surface glycan profiles by lectin array analysis revealed that α2-6sialic acid is expressed at very low levels on the cell surface of mCBSCs compared with that on mMSCs. In contrast, the lactosamine (Galβ1-4GlcNAc) structure, poly lactosamine- or poly N-acetylglucosamine structure, and α2-3sialic acid on both N- and O-glycans were more highly expressed in mCBSCs. Moreover, we found that mCBSCs secrete a greater amount of TGF-β1 compared to mMSCs, and that the TGF-β1 contributed to the self-migration of mCBSCs and activation of fibroblasts. Together, these results suggest that unique characteristics in mCBSCs compared to mMSCs may lead to advanced utility of mCBSCs for cardiac and noncardiac repair.
与小鼠间充质干细胞 (mMSC) 相比,新建立的小鼠皮质骨干细胞 (mCBSC) 是独特的干细胞。据报道,心肌梗塞后 mCBSC 治疗的心脏在心肌结构和功能方面有更大的改善。在这项研究中,我们检查了 mCBSC 与 mMSC 相比的干性特征、细胞表面聚糖谱和旁分泌功能。干性分析显示mCBSCs的自我更新能力大于mMSCs;然而,mCBSCs 的分化能力仅限于三种细胞(脂肪细胞、成骨细胞、软骨细胞)之间的软骨细胞谱系。通过凝集素阵列分析的细胞表面聚糖谱显示,与 mMSCs 相比,α2-6 唾液酸在 mCBSCs 细胞表面的表达水平非常低。相比之下,N -乙酰氨基葡萄糖结构和N - 和O -聚糖上的 α2-3 唾液酸在 mCBSC 中表达更高。此外,我们发现与 mMSCs 相比,mCBSCs 分泌更多的 TGF-β1,并且 TGF-β1 有助于 mCBSCs 的自我迁移和成纤维细胞的激活。总之,这些结果表明,与 mMSCs 相比,mCBSCs 的独特特征可能导致 mCBSCs 用于心脏和非心脏修复的高级效用。
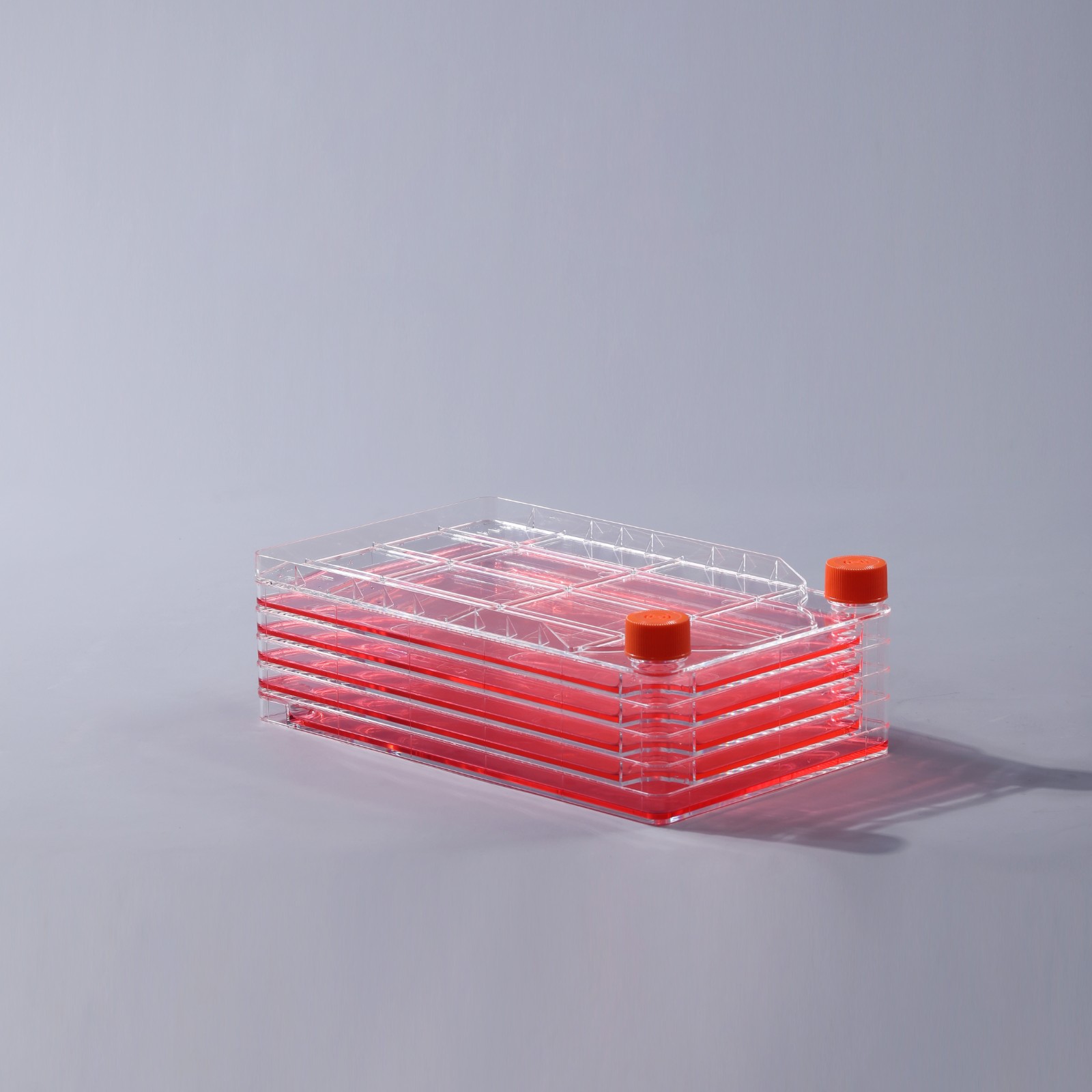
5层细胞工厂
Several cardiovascular diseases (CVDs) are the leading cause of death globally due to their high morbidity and mortality rates [1]. In the coming decades, the incidence of CVD caused by ischemic CVDs, such as myocardial infarction (MI), is expected to be in upward trend [2]. After MI, myocyte death and the reduction in the number of functional cardiac myocytes ultimately leads to heart failure. Until now, although there is scientific progress and advancements in surgical techniques, drugs and surgical treatments can only delay the progression of chronic heart disease, but not improve the function of infarcted myocardial cells [3]. Therefore, the use of stem cells has emerged as a promising treatment for heart disease [4]. Our research and others suggest that stem cells hold immense potential for cardiac repair and regeneration [5,6,7,8]. Clinical use of adult somatic stem cells (SSCs) is a reality today and many stem cell types, including bone-marrow-derived mesenchymal stem cells (MSCs) [9], bone marrow cells [10,11], cardiac-derived cardiac progenitor [12], and cardio-sphere-derived cells [13], have been tested. The beneficial effects of tested cell therapies on cardiac structure and function have been modest, and most studies to date have not been adequately powered to document efficacy. The emerging consensus from these studies suggests that the donated stem cell population falls short of fully restoring normal cardiac functional capacity because of a combination of issues, such as poor survival, lack of proliferation, engraftment, and differentiation. In addition, it seems that much of the benefit derived from cell therapy has come from the release of paracrine factors acting on the host myocardium rather than from differentiation of infused/injected stem cells into new cardiac tissue.

血清培养基瓶1000ml
几种心血管疾病 (CVD) 因其高发病率和死亡率而成为全球主要的死亡原因 [ 1 ]。在未来几十年中,由缺血性心血管疾病(如心肌梗塞(MI))引起的心血管疾病的发病率预计呈上升趋势[ 2 ]。MI 后,心肌细胞死亡和功能性心肌细胞数量减少最终导致心力衰竭。迄今为止,虽然手术技术有科学进步和进步,但药物和手术治疗只能延缓慢性心脏病的进展,而不能改善梗死心肌细胞的功能[ 3 ]。因此,干细胞的使用已成为一种很有前景的心脏病治疗方法 [ 4]]。我们的研究和其他人认为,干细胞保持心脏修复和再生[巨大潜力5,6,7,8 ]。临床使用成年的成体干细胞(SSCS)是今天,许多干细胞类型,包括骨髓来源的间充质干细胞(MSC)[现实9 ],骨髓细胞[ 10,11 ],心脏来源的心肌祖[ 12 ] 和心脏球衍生细胞 [ 13 ]],已经过测试。经过测试的细胞疗法对心脏结构和功能的有益影响不大,而且迄今为止的大多数研究都没有足够的效力来证明疗效。这些研究的新共识表明,由于存活率低、缺乏增殖、植入和分化等问题,捐赠的干细胞群无法完全恢复正常的心脏功能。此外,细胞疗法的大部分益处似乎来自作用于宿主心肌的旁分泌因子的释放,而不是来自注入/注射的干细胞分化为新的心脏组织。
上一篇: 离心管的材质介绍
下一篇: 细胞培养瓶使用注意这三点